Everything you need to know about perimenopause
6 months ago
Perimenopause6 months ago
Perimenopause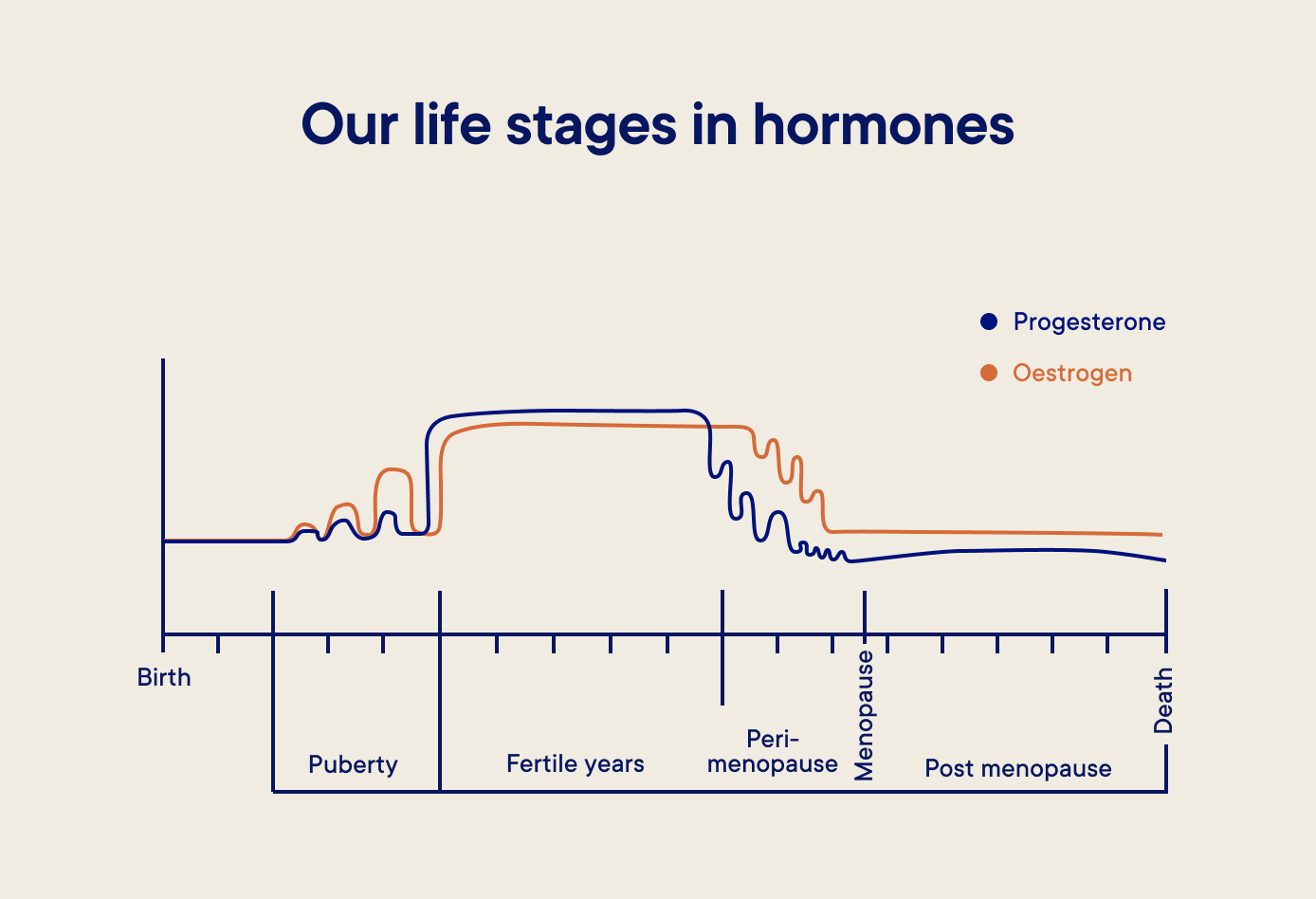
Over 1 billion women around the world will have experienced perimenopause by 2025, but it still seems to be shrouded in mystery. To cut through the confusion, we speak to three of our favourite women’s health experts about why we experience perimenopause, what to expect and what we can do to ease some of the common symptoms…
Reviewed by: Dr Bella Smith, Baz Moffat and Dr Emma Ross.
Talking about both menopause and perimenopause has been taboo for too long. But they’re finally getting the air time they deserve thanks to Davina McCall and her ground-breaking documentary, Sex, Myths and the Menopause ; former First Lady, Michelle Obama , who candidly shared a story about a time she had a hot flash on Marine One; and Hollywood celebs, such as Goop founder Gwyneth Paltrow , who talked openly about her experience of perimenopause on her brand's podcast.
“I think that when you get into perimenopause, you notice a lot of changes. I can feel the hormonal shifts happening, the sweating, the moods—you’re all of a sudden furious for no reason,” says Gwyneth.
Despite this crop of celebrities putting perimenopause and menopause into the spotlight, there’s still confusion around the difference between the two. Here, we chat to NHS GP, Dr Bella Smith; Baz Moffat, women’s health and fitness coach, and physiologist, Dr Emma Ross to explain everything you need to know about perimenopause.
“Although people tend to use the terms interchangeably, there’s a marked difference between perimenopause, menopause and post-menopause,” says NHS GP, Dr Bella Smith .
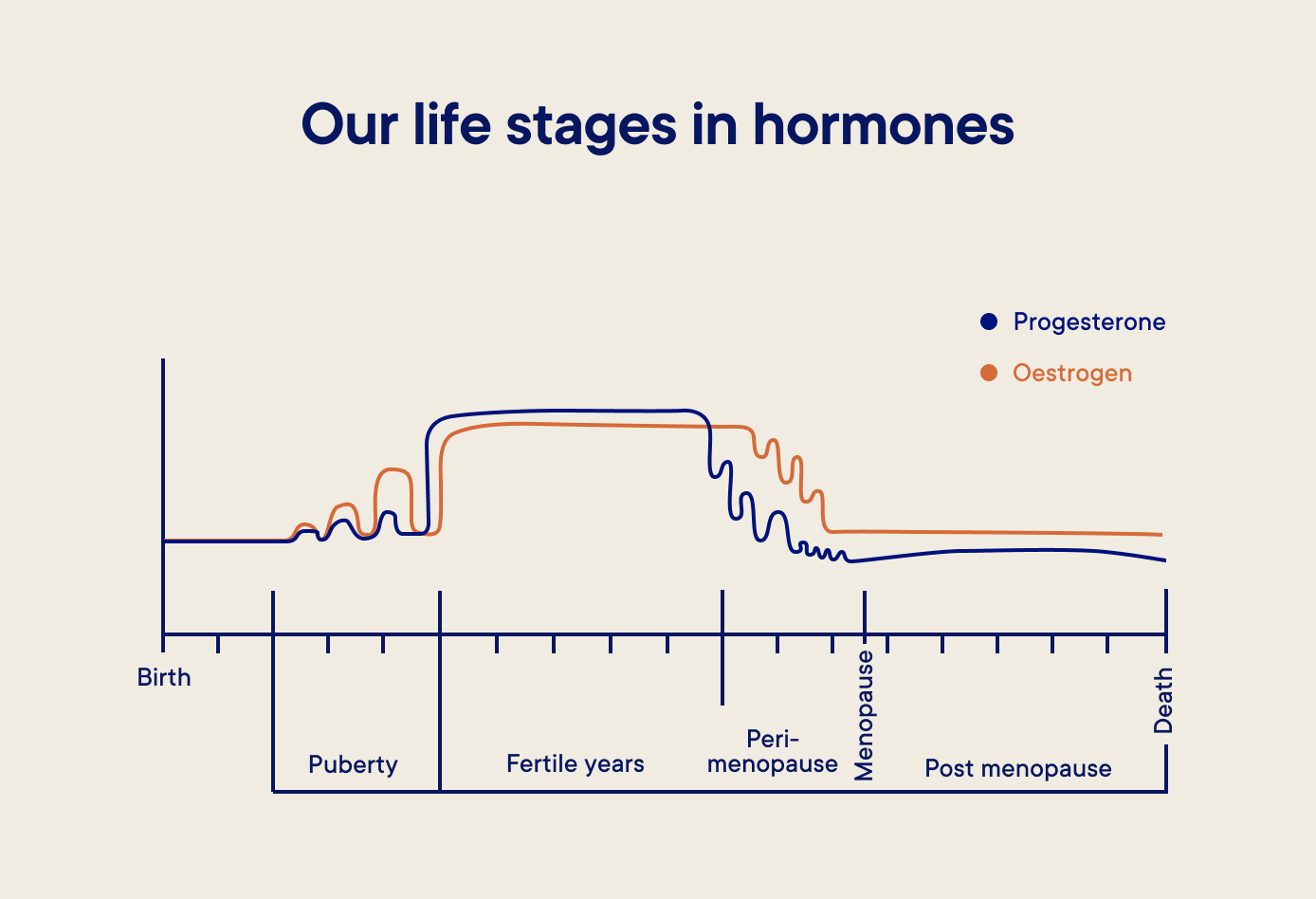
“The perimenopause is the transition time leading up to the menopause and is what I call, ‘the hormonal rollercoaster. This can be very unpredictable and chaotic and is characterised by a range of symptoms that occur because the oestrogen and progesterone you’re producing is rising and falling far more unevenly than it was, with a general decline in both hormones over time.”
“Some people are in perimenopause for only a short time - from a few months to a year. But for many, it lasts up to a decade,” adds Baz Moffat, women’s health and fitness coach .
Menopause, in contrast, occurs when you’ve stopped producing the hormones that cause your period (oestrogen and progesterone) and have gone without a period for 12 months if you’re over 50, or two years if you’re between the ages of 45 and 50. “After this time, you enter ‘post-menopause’,” says Dr Bella.
“Because of this confusion, often when people are referring to the menopause, they are probably talking about post-menopause.”
To be super clear, then…
- Perimenopause is... the transition time when your main menstrual cycle hormones are declining and probably becoming erratic, but your periods haven’t finished.
- Menopause is... the marker when you haven’t had a period for 12-24 months (depending on your age).
- Post-menopause... is the time after that menopause
In the same way that our periods start at very different times, the path through perimenopause can be completely different from woman to woman, with different lengths and different symptoms.
Usually, perimenopause starts in your mid-40s (with the oft-cited average age being 47.5), but it may begin as early as your mid-30s or as late as your mid-50s.
“The other thing to note is that people can actually come in and out of perimenopause, and their periods can stop and start,” says Bella. “As an example, we saw many women having perimenopausal symptoms during COVID because of stress. Once stress levels then settled down, they went back to having a normal cycle, and they no longer had perimenopausal symptoms.”
“Because your hormones are changing constantly during perimenopause, there is no simple blood test to tell you that you’re definitely perimenopausal. But there are lots of physical signs and clues that a GP will use to diagnose you.
“If you’re in your 40s and you notice that sleep starts to go,” says Baz, “you find it difficult to regulate temperature at night, your cycle starts to change length or your body feels like it’s changing, this suggests you could be going through perimenopause.”
Perimenopause isn’t all doom and gloom. Because our health suddenly comes into focus, it can be a stage in life where women prioritise themselves for the first time in decades
Reducing oestrogen levels
Oestrogen’s main role is to regulate the menstrual cycle, so as your cycle begins to wind down during the perimenopause, your oestrogen levels also start to decline.
Because this declining oestrogen isn’t gradual or smooth and can spike and crash on its way down, it can cause perimenopausal symptoms, such as hot flushes, vaginal dryness, brain fog and irritation - or the red mist, as it’s affectionately nicknamed by Dr Bella.
“Because oestrogen is also linked to levels of the good-mood hormone, serotonin, in the brain,” says Dr Emma Ross, Jennis physiologist, “when our levels of oestrogen go down, so do the levels of serotonin.” It’s because of this that you may feel low, tearful or depressed.
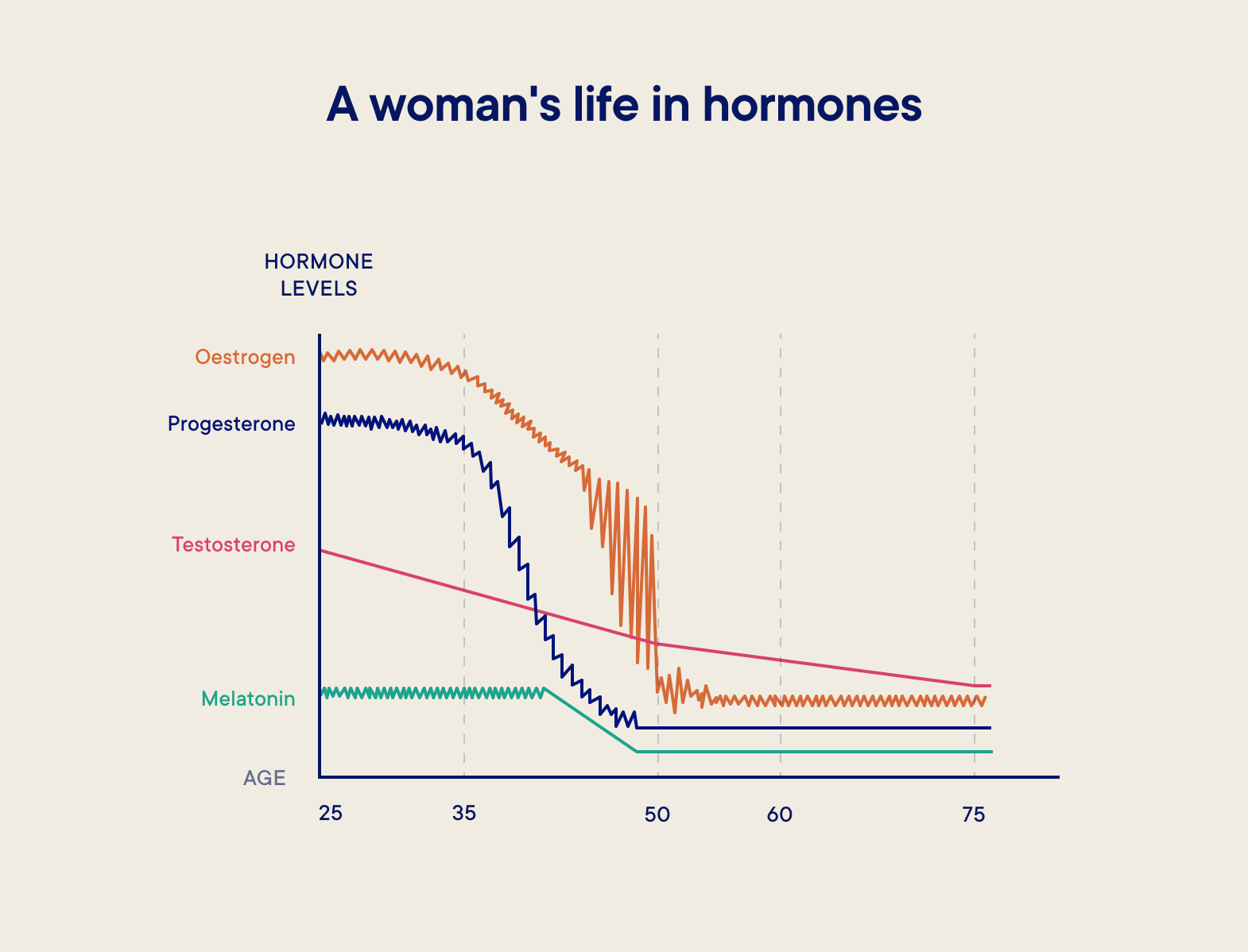
Reducing progesterone levels
“You produce progesterone when you ovulate,” explains Dr Emma, “so when you go through perimenopause and stop ovulating, your progesterone levels also decline.” Because progesterone has a calming effect on the body, decreasing levels could contribute to poor sleep, irritability and anxiety.
Reducing testosterone levels
Although testosterone is often overlooked in women (and often deemed to be a male hormone), we actually produce three times as much testosterone as oestrogen before the menopause - and it’s testerone that drives our libido.
The decline in testosterone in women is solely age-related, not menopause-related, and begins years before perimenopause. But low testosterone can lead to things like low libido, weight gain and changes in mood and motivation.
“The one thing I want to stress before we talk more about symptoms and symptom relief,” says Dr Bella, “is that perimenopause isn’t all doom and gloom. Because our health suddenly comes into focus, perimenopause can be a stage in life where women actually take control of their health and prioritise themselves for the first time in decades.
“If you think about your job, family, house and all the things that you are juggling at this age, we’re often so busy that we forget to prioritise ourselves, so this is often a great time to wipe the slate clean and prioritise the things you’ve been meaning to do but have been too busy for, such as exercise, healthy eating and so on.”
“In the same way that there are over 150 pre-menstrual symptoms, there are probably just as many - if not more - perimenopausal symptoms,” says Dr Emma. “Because they show up in different women in different ways, the key is to be able to list yours and be really clear about what’s happening and when they’re showing up, which is where a tracker can help .” Some common symptoms include:
Irregular periods, spotting or heavier bleeding
‘With your oestrogen and progesterone levels peaking and troughing, you may notice your cycle begin to shorten, become more irregular or even heavier at times,’ says Dr Emma. “Changes in your cycle are probably one of the first things to look out for.”
Hot flushes and night sweats
Around 80% of women will experience hot flushes at some point during perimenopause, and research has proven this is usually the main culprit for sleeping difficulties and feelings of exhaustion.
Difficulty losing weight
You might notice that the things that you usually do to maintain a healthy weight aren’t as effective as they used to be and it may be tougher to get rid of belly fat in particular.
Lower libido and vaginal dryness
Decreasing levels of our sex hormones can affect our sex drive, how often we feel aroused and also cause vaginal dryness and thinning of the vaginal wall (known as vaginal atrophy).
Problems with memory or concentration
Decreasing oestrogen levels affect our cognition and can lead to a feeling of brain fog – not being able to find the right words or forgetting things, which can feel really worrying and frustrating.
Irritability and low mood
The peaking and troughing of our hormones can affect our mood, giving rise to shorter patience and irritation. In addition to this, we can experience general anxiety as a result of worrying about our changing bodies and symptoms.
Urinary weakness
We have oestrogen receptors all over our body, and the vagina and urinary tract are particularly dense in these. ‘As the levels of the oestrogen hormone decrease, you might experience urinary stress incontinence,” says Baz. “Even if you haven’t had children, you may find your pelvic floor feels weaker, which is why fitting pelvic floor exercises into your fitness routine is so important.”
Exercise is a proven intervention for easing some perimenopause symptoms, but eating well and avoiding or reducing things that can contribute to anxiety or poor sleep, such as caffeine and alcohol can also help.
With your body more prone to cortisol (the stress hormone) storage during perimenopause, it’s important to look at your lifestyle and see where you can add activities or exercise that help you to destress, while bringing you joy. Whether that’s riding your bike, walking the dog, massages, meditations, breathwork - anything that actively helps you switch off and relax.
Strength training fires up the metabolism, which is helpful if you're trying to shift weight or belly fat
Our bone health and muscle strength begin to decrease during your 30s, but it really declines when oestrogen leaves the system.
“Strength training and impact work like weight training or bodyweight exercises can slow and even negate the decline” says Baz. “It’s also fantastic for firing up our metabolism post-session, which is helpful if you’re trying to shift weight or belly fat."
The caveat here is to make sure you don’t start overdoing your exercise activities and then push your body into a stressful state, as this can dial up the stress levels we want to keep in check.
It’s ok to go hard or do a HIIT, to do that long endurance run or really sprint at the end of the ParkRun , but whenever you push yourself and your body, you need to leave time to wind down physically and hormonally, so that you don’t add stress to your system.
“Exercise that involves hand-eye coordination or fires up your mental acuity like squash drills, boxing combos or simply counting backwards as you squat, can help to combat the brain fog and help you feel mentally sharp,” says Baz.
Not only does it help you dial up your body awareness, but intentional pelvic floor exercises also help to combat the decline of oestrogen receptors in your vagina, helping to stave off incontinence or prolapse symptoms. “You usually need to be taught specific exercises, so speak to a doctor or physiotherapist, and try incorporating them into your exercise routine,” says Baz.
Read our in-depth article about symptoms and the things that can help here
If lifestyle strategies still aren’t working for you, don’t be afraid to go for interventions. “It’s important to remember that struggling at this lifestage isn’t a sign of weakness,” says Baz. “If you’re significantly impacted by perimenopausal or menopausal symptoms, you may not be able to navigate it just with lifestyle alone and it’s ok to seek out medical intervention.”
Here are some of the most common ones:
Hormone replacement therapy (HRT)
HRT is one of the most common treatments for peri and menopause and relieves symptoms by replacing oestrogen. You can take it via tablet, gels or patches.
Localised oestrogen
For vaginal dryness, which can cause pain during sex, localised oestrogen creams and lubricants can help.
Talking therapy
If you’re struggling mentally, a doctor might refer you to talking therapy to help you process your feelings and experiences. One of the most common types is cognitive behavioural therapy (CBT), which can help with low mood and anxiety.
Dr Emma, Baz and Dr Bella are the experts behind The WellHQ
 Cycle syncing
Cycle syncing Perimenopause
Perimenopause Perimenopause
Perimenopause Perimenopause
PerimenopauseSign up to learn everything you need to know about CycleMapping, plus how you can live better and feel better through optimising your fitness to you.
This website uses cookies to ensure you get the best experience on our website. Learn more

Sign up for the very latest news on women's fitness, health and hormones, plus be the first to receive exclusive offers and extras